Complete tumor resection is a critical aspect of cancer treatment. For many cancers, though, complete resection is very difficult to achieve. One major hindrance is the inability to distinguish diseased from non-diseased tissue. Surgery guided by near-infrared fluorescent optical probes is emerging as a promising advancement in surgical methodology, enabling surgeons to better visualize diseased tissue, resect tumors completely, and ultimately improve patient outcomes. For a probe to be an effective surgical aide, it must be highly specific to the target. In other words, the probe must bind only to diseased tissue and should bind to it with a high affinity. This creates a highly-contrasted tumor-to-background ratio, which enhances both intraoperative in situ tumor visualization and ex vivo histopathological evaluations of tissue sections.
Mode of image capture is another important consideration for near-infrared (NIR) fluorescent optical probes as surgical aides. Several imaging modalities exist, and each serves a unique purpose. Positron Emission Tomography (PET) and Single-Photon Emission Computed Tomography (SPECT) allow for imaging of deep tissues and organs, bones, and inside the ribcage, but cannot be used intraoperatively. NIR fluorescence, on the other hand, is most effective for shallow tissue and organ imaging, and can be used real time during surgery to guide tumor resection. IRDye fluorescent dyes can be conjugated to compounds used in various modalities, and combining modalities can be very powerful for probe validation.
Dual Modality Tagging with IRDye 800CW-NHS Stained Monoclonal Antibodies and Radioactive Tracers Provide Greater Insight into Tumor Characteristics
A 2011 study published in the Journal of Nuclear Medicine by Terwisscha van Scheltinga et.al. demonstrates the power of combining imaging modalities with IRDye conjugates. This pre-clinical mouse study investigated the potential ability of targeted monoclonal antibodies to deliver fluorophores to specific tumors for surgical resection. The antibodies in question were bevacizumab and trastuzumab. Bevacizumab is an anti-vascular endothelial growth factor (VEGF) monoclonal antibody and trastuzumab is an anti-human epidermal growth factor (HER) 2 monoclonal antibody. Each was stained with IRDye 800CW NHS ester for NIR fluorescent imaging, and were then combined with 89Zr-labeled radioactive tracers for PET imaging.
Tumor uptake of the IRDye dye-conjugated antibodies was compared against uptake in the 89Zr-labeled counterparts in mice with VEGF- and HER2-overexpressing tumors. Tumor-background ratio (TBR) was assessed for specificity, and the results were promising: “The excellent selective tumor uptake” of the 89Zr-labeled IRDye tracers imaged with PET “was also observed for the same antibodies labeled with a fluorescent dye” [1]. With the specificity of the dye-conjugated antibodies validated in tissue analysis, the authors performed intraoperative imaging of the same VEGF- or HER2-expressing tumor lesions, concluding that “In a preclinical setting, NIR fluorescence-labeled antibodies targeting VEGF or HER2 allowed highly specific and sensitive detection of tumor lesions in vivo” [1]. Lastly, this study demonstrates how combining PET and NIR fluorescence imaging may be used to validate the specificity of a dye-antibody conjugate ex vivo prior to intraoperative imaging.
Cetuximab-IRDye 800CW Conjugated Probes Target EGFR for Intraoperative Surgical Navigation of Head and Neck Squamous Cell Carcinoma
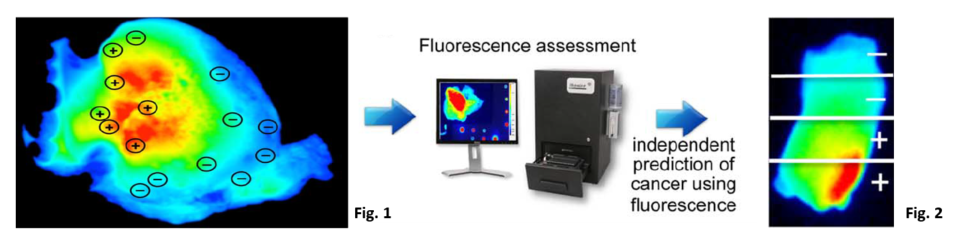
A 2015 study published in Clinical Cancer Research by Rosenthal, et.al. demonstrates the clinical potential of IRDye 800CW as a tumor-specific contrast agent in cancer surgery. Twelve patients participated in a dose-escalation study of cetuximab, an anti-EGFR monoclonal antibody, conjugated to IRDye 800CW. Over 90% of head and neck squamous cell carcinoma tumors overexpress EGFR, which presents an opportunity for EGFR-targeted antibodies as a vehicle for IRDye fluorophores [2]. Wide-field NIR imaging was used intraoperatively and multiple tissue sections were collected and imaged in the Pearl Impulse imaging platform (LI-COR Biosciences). These results were also promising:
- Fluorescence imaging of the primary tumor in situ demonstrated high average tumor to background ratio. The authors noted that “fluorescence imaging provided robust contrast between tumor and surrounding tissue” [2].
- Fluorescence in confirmed tumor tissue imaged ex vivo was significantly greater (P<0.001) than non-cancerous tissues, validating the preferential uptake of IRDye 800CW conjugated monoclonal antibodies in diseased tissues [2].
- No Grade 2 or higher treatment emergent adverse effects occurred, and IRDye 800CW-cetuximab was reported to be “well tolerated” by participants, corroborating the positive results of IRDye 800CW pre-clinical toxicity studies [2].
The authors conclude “this optical labeling technique could be safely applied to other protein-based therapeutics to confirm successful targeting or assess off-target activity during early phase trials” [2].
Conclusion
Near infrared fluorescent optical imaging with dye-conjugated tumor-specific antibodies is quickly emerging as a viable intraoperative tool for cancer surgery. For an optical probe to be successful, it must be highly specific to the target tumor and bind strongly to create high tumor to background ratio. In recent pre-clinical studies, IRDye 800CW NHS ester has shown equal or better tumor to background ratio than established PET methods with nuclear-tagged probes. In similar clinical studies, IRDye 800CW has demonstrated high tumor to background ratio in humans intraoperatively for tumor excision. For more exciting clinical applications of IRDye, please visit the Optical Probe Development and Molecular Activity Measurement web pages.
References
- Terwisscha van Scheltinga, A.G.T., et al. Intraoperative Near-Infrared Fluorescence Tumor Imaging with Vascular Endothelial Growth Factor and Human Epidermal Growth Factor Receptor 2 Targeting Antibodies J Nucl Med 2011; 52:1778–1785. doi: 10.2967/jnumed.111.092833.
- Rosenthal, E.L., et al. Safety and Tumor-specifity of Cetuximab-IRDye800 for Surgical Navigation in Head and Neck Cancer. Clin Cancer Res 2015, Aug; 21(16):3658-3666. doi: 10.1158/1078-0432.CCR-14-3284.
- Ahn BC. Sodium Iodide Symporter for Nuclear Molecular Imaging and Gene Therapy: From Bedside to Bench and Back. Theranostics 2012; 2(4):392-402. doi:10.7150/thno.3722.
Powered by Froala Editor