Coronavirus Research Part 1: Understanding SARS-CoV-2 and the human host response
Our three-part series on the massive world-wide research response to the COVID-19 pandemic will first look at how we came to better understand the virus and the human host response. Part 2 will cover research into potential diagnostics and vaccines for SARS-CoV-2. Part 3 will be about the therapeutic targets, neutralization antibodies, and inhibitors that could end the pandemic.
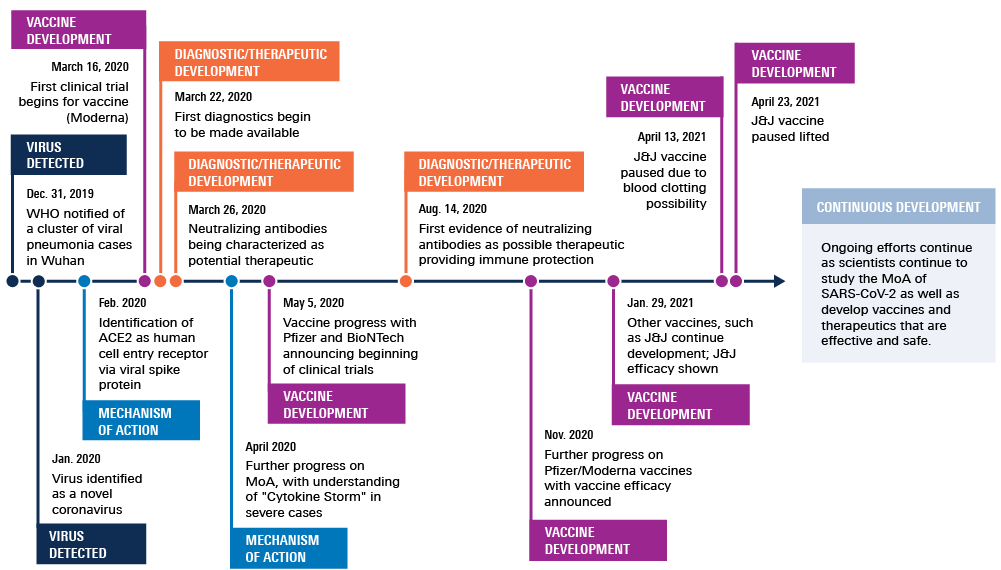
Following the initial identification of a pneumonia-like respiratory disease in late 2019, scientific knowledge about the novel coronavirus has surged, despite the worldwide shut down of nearly every sector of life and society. In fact, the COVID-19 pandemic has necessitated a massive global research undertaking to understand how SARS-CoV-2 works and how the human host responds to it.
The SARS-CoV-2 doorway into human cells
The frenetic pace of scientific research and the resulting avalanche of SARS-CoV-2-related pre-print and peer-reviewed publications have all contributed to the still-growing foundation of scientific understanding of how the virus works, including learning how SARS-CoV-2 is able to invade the human body so successfully. As is typical for a coronavirus, the outer layer of SARS-CoV-2 is covered in sharp protein spikes that stick out from the surface of the virus. Previous research on SARS-CoV – which caused a global outbreak of severe acute respiratory syndrome in North America, South America, Europe, and Asia in 2003 – had already identified how the coronavirus spike protein attached to its host’s cell membrane to gain entry into the cell: The spike on the outer layer of SARS-CoV binds with ACE2, an enzyme found on the surface of many cell types. ACE2 was known as the doorway for SARS-CoV into human cells.
Building on that existing knowledge, colleagues at the Institut Pasteur in France and the University of Washington and Fred Hutchinson Cancer Research Center, both in Seattle, were able to add to the understanding of the mechanism of action for SARS-CoV-2. With fluorescent Western blotting using Alexa Fluor 680 and an Odyssey CLx Imaging System, the international research group demonstrated in a paper published by Cell in March 20201 that both SARS-CoV-2 and SARS-CoV spike proteins bind to human ACE2 similarly, which leads to their efficient spread. Additionally, their work distinguishes how SARS-CoV-2 is different from SARS-CoV because of a distinctive furin cleavage site. With this understanding, they were able to not only begin characterizing the structure of SARS-CoV-2 to act as a blueprint for the design of vaccines and antivirals but also to identify some antibodies that could inhibit entry of SARS-CoV-2 into cells.
Suppressing the antiviral response and initiating a cytokine storm
Along with understanding how the novel coronavirus invades cells, research from a group at the Chinese Academy of Medical Sciences and Peking Union Medical College, both in Beijing, identified specifically how SARS-CoV-2 suppresses the antiviral response so it can infect its host. Their paper, published February 2021 in Cellular and Molecular Immunology, describes their use of Western blots and an Odyssey CLx Imaging System2 to identify the mechanism of the suppression in more detail, and they conclude that the invading virus can antagonize its host’s antiviral innate immune response.
New research in the last year has also explored the human immune system’s surprising response to COVID-19 infection. In another Cell publication, made available online in May 2020, researchers from the Icahn School of Medicine at Mount Sinai and Weill Cornell Medicine, both in New York; the Stanford University School of Medicine in Stanford, CA; and the Chan Zuckerberg Biohub in San Francisco explain how they used Western blotting and the Odyssey CLx Imaging System as part of a study that recorded the “unique and inappropriate inflammatory response” induced by SARS-CoV-2. This response, they write in their paper3, is characterized by low levels of two types of interferons coupled with elevated cytokines. They propose that reduced innate antiviral defenses combined with overabundant cytokine production – called a “cytokine storm” – define and drive the symptoms of COVID-19.
World-wide research response quickly advances understanding of SARS-CoV-2
The moment COVID struck, the global scientific community responded with overwhelming speed to provide the research and data that would be needed to address the spreading pandemic. Here, we’ve seen how research from three publications – including scientists at nine institutions on three continents – contributed to the basic understanding of the mechanism of action and host response to SARS-CoV-2. LI-COR technology was used for Western blots in this world-wide quest to understand the novel coronavirus and the human response to it. Why not check into what LI-COR can do for your research?
References
- Walls, A. C., Park, Y.-J., Tortorici, M. A., Wall, A., McGuire, A. T., & Veesler, D. (2020). Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell, 181(2), pp 281-292.E6. DOI: 10.1016/j.cell.2020.02.058
- Wang, W., Zhou, Z., Xiao, X., Tian, Z., Dong, X., Wang, C., et. al. (2021). SARS-CoV-2 nsp12 attenuates type I interferon production by inhibiting IRF3 nuclear translocation. Cellular & Molecular Immunology, 18, pp 945-953. DOI: 10.1038/s41423-020-00619-y
- Blanco-Melo, D., Nilsson-Payant, B. E., Liu, W. C., Uhl, S., Hoagland, D., Møller, R., et.al. (2020). Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell, 181(5), 1036-1045.e9. DOI: 10.1016/j.cell.2020.04.026
Powered by Froala Editor